Moderna and Pfizer Challenge the Status Quo with New mRNA Vaccine Approach
November 23, 2020
- Until now, the majority of vaccines have been developed using a conventional method of stimulating the body’s immune response
- Moderna and Pfizer are the first to use mRNA technology to develop a vaccine against COVID
- Both companies have shown >95% efficacy for their vaccine candidates in phase 3, with trials still ongoing
Things are finally starting to look up as biotechnology company, Moderna, found a 94.5% efficacy of their vaccine candidate against COVID. The phase 3 trial of mRNA-1273 is still ongoing but the company plans to file for Emergency Use Authorization (EUA) in the USA. Pharmaceutical company, Pfizer, also came out with data regarding their drug candidate and similarly found >95% efficacy.
Both companies are the first to use mRNA technology to develop a COVID vaccines, whereas traditional ones use weakened or inactive forms of the disease. While vaccines in the past have taken years to develop, Moderna and Pfizer were able to do so within months. The question is whether their success can be chalked up to this new technology?
Vaccine Technologies Have Remained Unchanged Until Now
The body itself acts as a particularly good defense against most pathogens. Physical barriers like skin and mucous membranes physically protect against germs entering the body. However, in the event that a pathogen does enter, the body’s immune system is triggered and attacks. Parts of the pathogen, called antigens, are recognized by the immune system as foreign, and lead to the production of antibodies.
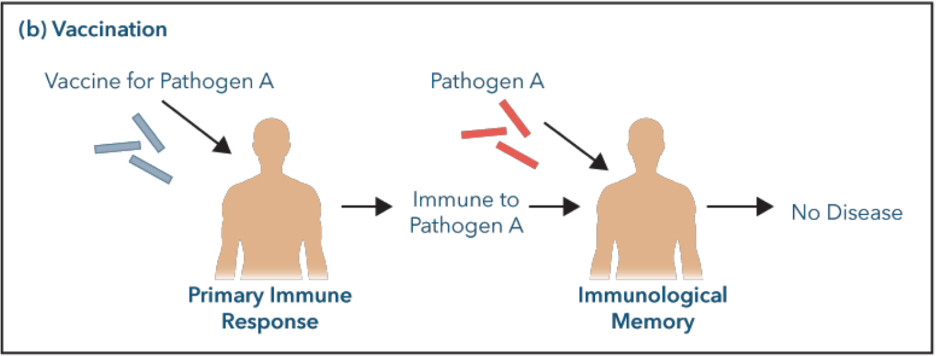
In the event that the pathogen is encountered again, the body has already developed memory antibodies. They recognize and remember the pathogen and are thus able to mount an immune response that is even quicker and stronger than the first (memory response).
Conventional vaccines essentially work by mimicking the body’s natural response to a pathogen. Their goal is to prevent disease by deliberately exposing the immune system to a non-pathogenic or inactive form of the disease. Patients are injected with a small dose of the virus to “prepare” the immune system. In response, the immune system will create antibodies to fight off the foreign virus injected by the vaccine and thus, create a memory response the first time a pathogen is encountered. This way, the second time that same virus is encountered, the immune system will have natural immunity (see image below).
This has been the main method of vaccine development for the past several decades. It is a difficult and lengthy process with several steps involved. The vaccine needs to be developed, undergo pre-clinical and clinical testing, approval, manufacturing and control once out on the market. This whole process is very tedious and usually takes several years to complete. Though all vaccines come with potential side effects, this method has been the most widely used and accepted.
Many companies, like AstraZeneca, used this same mechanism to attempt developing a COVID vaccine but were faced with safety concerns along the way. Moderna and Pfizer were two pilot companies to challenge the status quo and attempt a COVID vaccine using mRNA.
mRNA Basics
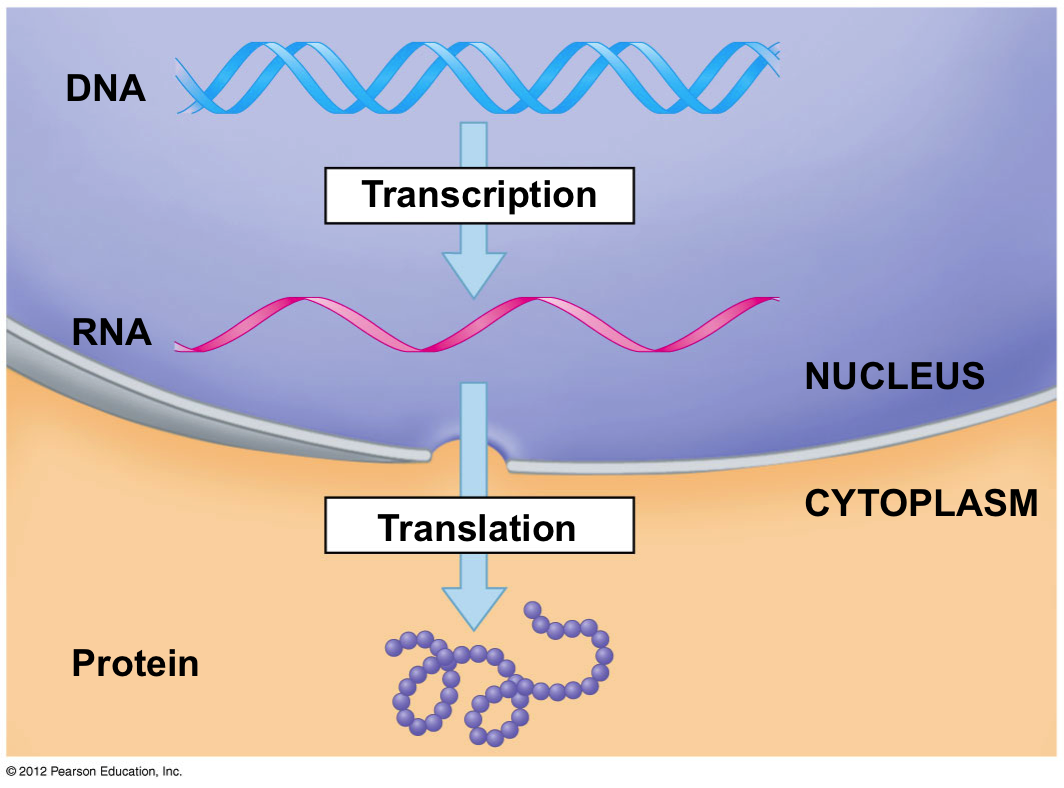
Messenger RNA (mRNA) is a type of RNA that contains the information cells need to make certain proteins. Cells use RNA to make proteins whose functions are to build and repair things in the body, just to name a few. Scientists manipulated this process and used it to develop a COVID vaccine.
Think of it this way: DNA is the “instruction manual” and mRNA is the messenger that takes a replicated copy of those instructions to the location in the cell where the “workers” are. The workers use the instructions to create the protein, which is used as a defense against foreign objects.
Importance of Spike Proteins Found on COVID
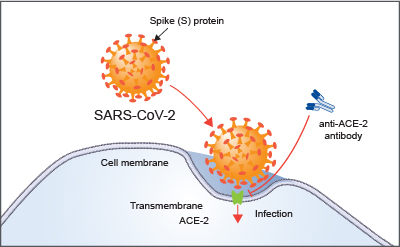
SARS-Cov-2, the virus that causes COVID-19, contains spike proteins on its surface. These spike proteins bind to human cells to penetrate, enter, and infect the healthy cells of individuals (see image below). Although humans themselves do not have spike proteins, they are able to detect them and block this binding process with antibodies. Creating these antibodies is the objective of a vaccine, which we discuss next.
The Vaccine Process
To start the development process of the vaccine, scientists had to isolate the virus from an infected individual. It was then sequenced (similar to getting a word for word write-up of the genetic information of the virus) and kept in a public database. Since spike proteins are part of the virus, their exact sequence was included. This made creating synthetic spike protein “instructions” a possibility.
The idea behind Moderna and Pfizer’s mRNA vaccines was to replicate the sequence (instructions) of the spike proteins into synthetic mRNA and inject this into humans through a vaccine. That way, the body would recognize the injected mRNA and cells would generate a small amount of spike protein. Recall that although humans do not have spike proteins, they are able to recognize them. Therefore, the body’s immune system would detect the spike proteins and build immunity against them.
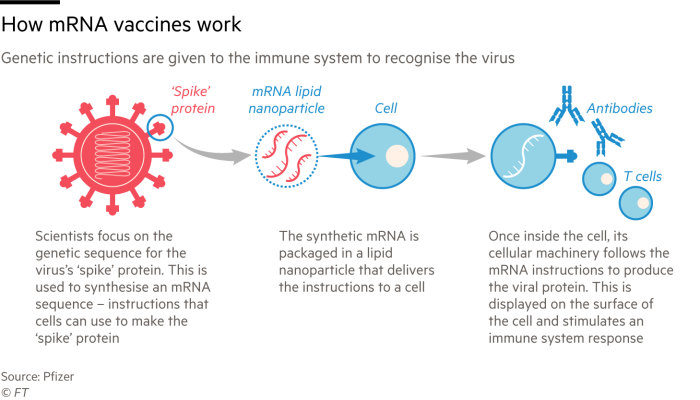
That is in essence, the function of a vaccine. To produce a strong and quick memory response prior to natural infection. The Moderna and Pfizer vaccine do just that. They prime the immune system with just enough synthetic mRNA-generated spike proteins so that protective antibodies are made. This way, if an immunized individual becomes infected with COVID, they will have a much stronger and quicker response.
The benefits of mRNA vaccines seem to far outweigh those of conventional vaccines for multiple reasons:
Efficacy: They shown to be over 95% efficacious for both companies with minimal safety concerns reported to date.
Production time: mRNA vaccines can also be produced in a fraction of the time, a major key when faced with a global pandemic. Unlike conventional vaccines that take years to develop, Moderna and Pfizer were able to make theirs in a span of months. This is because
Production safety: Traditional vaccines involve producing and collecting a large quantity of virus and subsequently growing and manipulating it in the lab. An weakened or inactive version of the virus is injected into the body. This process is time consuming and can be hazardous. For mRNA vaccines, you do not need to make the virus to make the vaccine. Instead, information about the virus (ie. its sequence) is used, replicated and administered into the patient using synthetic mRNA.
All of these beneficial aspects of mRNA vaccines can potentially make it a breakthrough during the COVID pandemic and for future disease outbreaks. Since both mRNA vaccines for Moderna and Pfizer were made in a short period of time and phase 3 trials are still ongoing, there is a need for more substantial data.
Questions regarding the long-term safety of the vaccines remain and are at the forefront of everyone’s mind. There is also a question of protection duration provided by the vaccines. Once antibodies against spike proteins are made, do they last indefinitely? Or do they dwindle down months later? Only time will tell.


