Possibility of COVID Re-infection Doesn’t Seem as Far Off as Originally Thought
August 31st, 2020
To date, we know that the body mounts an immune response to COVID when infected. What we do not know, though, is how long this immunity lasts and whether or not it protects from re-infection. Recently, the attention of many has been spiked at the news of a young 25-year old male being infected twice, with two genetically distinct strains of COVID.
Genetic sequencing data showed that the two infection events contained certain mutations that would classify them as distinct strains. However, since the patient was re-infected within a short 2-month timeframe of initial infection, it is unlikely that this can be explained through evolution. Scientists are still unsure of the exact mechanism, but based off of the information to date, it seems that reinfection with COVID is possible, but rare.
Evidence on the relationship between immunity and other strains of coronavirus show that immunity to the disease can be lost within 1-3 years. Public health experts usually expect that if the immune response to initial infection is not enough to protect from re-infection, it would at least dampen the symptoms the second time around.
What is so interesting about the case of the 25-year old male is that, compared to the first time the patient tested positive, his symptoms seemed to have worsened the second time with him even having to be admitted to the hospital for oxygen support.
Immunity Can Be Strong but Not Always Consistent
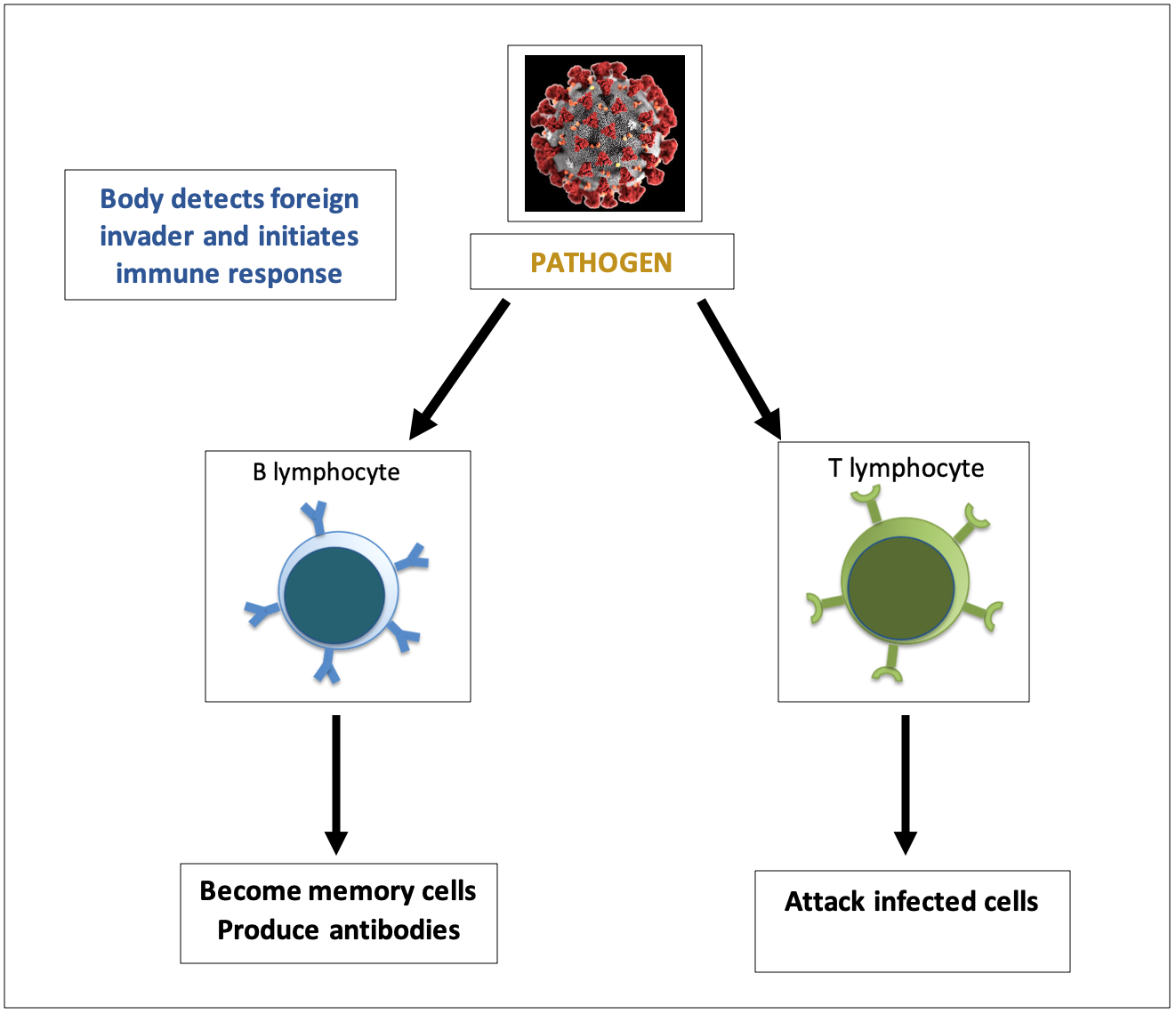
Normally, our immune system fights an infection by providing us with three main soldiers;
- Antibodies: molecules that attach to pathogens and block them from causing infection
- T-cells: attack infected cells and stop them from spreading
- B-cells: produce antibodies and memory cells that strengthen immune response the second time around
Problem is, with a new pathogen like COVID, until more data regarding the mechanism of its re-infection comes along, it is hard to tell how long the body’s immunity against it will last. However, like every mechanism in the body, no two people will have the same response to something. That goes for immunity too. The strong immune response a young healthy individual will mount to any given infection will not be the same as the much weaker one an older individual will produce. The severity of the disease will also produce differing immune responses in infected individuals. Someone with a severe case of COVID will likely produce a much stronger immune response compared to someone with a mild case.
Details regarding someone’s immunity can be seen through blood work. For infections that we are well acquainted with, scientists have a good estimate of what levels of antibodies/T-cells/B-cells need to be detected in the blood to know whether someone is protected. However, with a new virus like COVID, there is not enough data to establish such parameters. Because of this, it is hard to know if we build a strong enough immunity to fight off COVID and if it will last long enough to protect us from reinfection.
Inconclusive data complicates the development of a vaccine
The goal of a vaccine is to deliver a small enough dose of the pathogen to initiate an immune response strong enough to create memory cells. That way, if the individual is exposed to the pathogen at a later time, they will have a strong enough immunity to avoid disease. However, with the data we have so far, it seems as though initial exposure to COVID might not result in complete immunity. This can complicate the development of a vaccine that relies on this concept to be effective.


